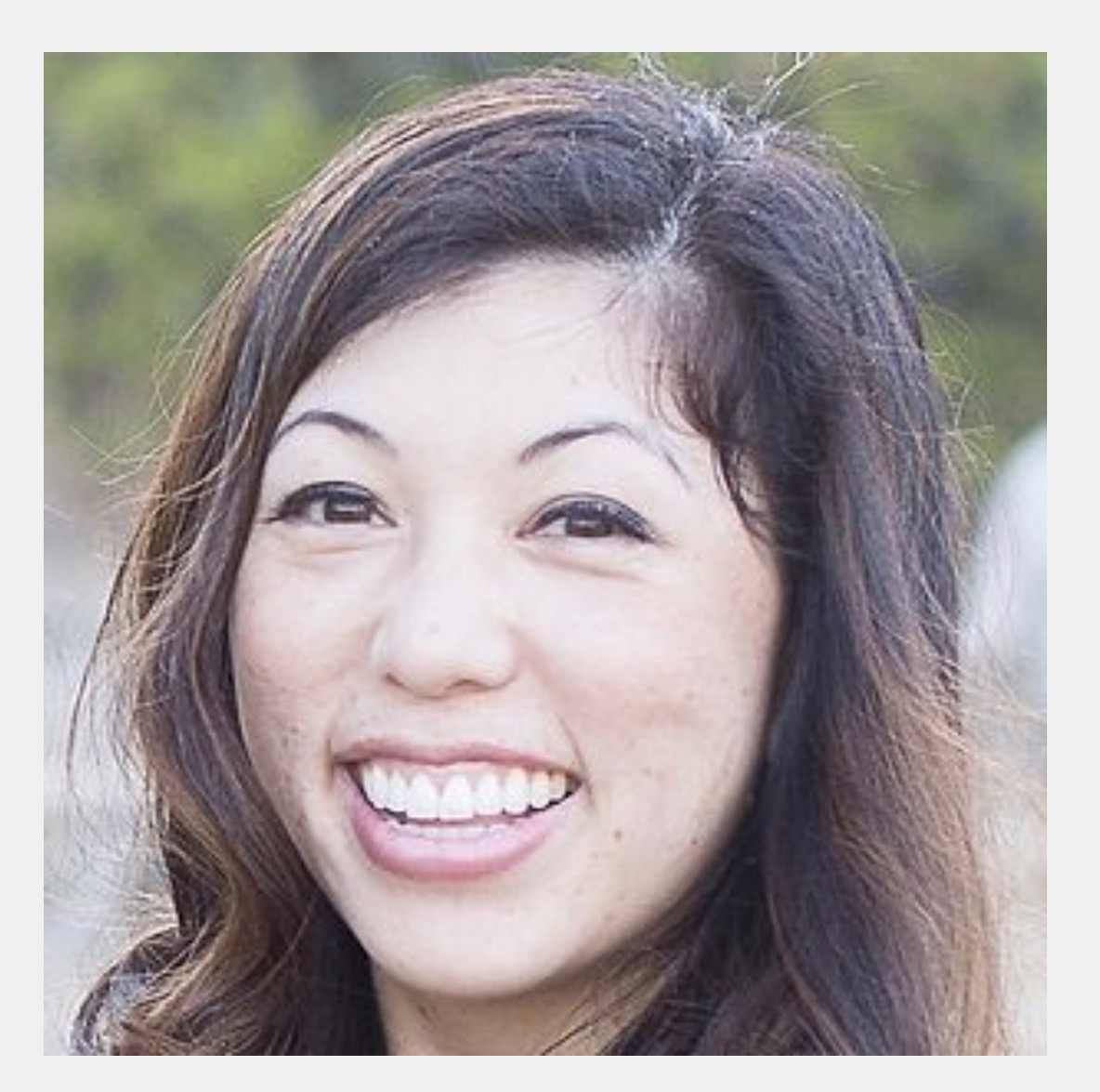
Episode 54: Dr. Jenna Silakoski (She/Her) of North Idaho DPC - Hayden, ID
- Maryal Concepcion
- Sep 5, 2021
- 36 min read
DPC Doctor

Dr. Jenna Silakoski, DO (who ETSd as a Major from the US Army in 2019) attended both undergraduate and medical school in Ohio where she went to Ohio University College of Osteopathic Medicine. Graduating in 2012 she dedicated herself to serving our nation as she immediately took an oath as an officer in the United States Army. Serving as a Soldier and a physician, she completed her residency at the Carl R Darnall Army Medical Center in Fort Hood, TX and became a Board Certified Family Physician in 2015. Since then she has attained the rank of Major and served in many roles including Medical Director of an outpatient clinic and Officer in Charge for the Family Medicine Residency Clinic at Fort Hood as well as providing care for Soldiers and their families across the spectrum “from cradle to grave.”
As early as medical school, Dr. Silakoski saw firsthand many of the challenges that existed with traditional healthcare both in the civilian world as well as the military. Difficulties with access to care and the lack of time able to be spent with patients left her searching for a better way. As Direct Primary Care surfaced as an answer to physician and patient’s alike calling for a way to bring quality-driven relationship-based care back into medicine without the complications of insurance, Dr. Silakoski seized the opportunity to bring care directly to her patients which she does at her DPC North Idaho DPC.
Dr. Silakoski raises her two young children, AJ and Everly, with her husband Ryan who works for a company that supports our military. She enjoys painting, exploring the world with her family and continues to pursue her dreams in the community of North Idaho.
In today's episode, Dr. Silakoski shares her experience practicing medicine in both the civilian and military worlds and how she makes her dream of providing relationship-based care and having time with her patients at her DPC North Idaho DPC. Hear her share her story as to how she ended up in Idaho and how she has grown her practice to the point she is adding on another physician in the fall!
------------------------------------------------
Dr. Silakoski's FB post with her clinic data (reproduced with her permission)
"For anyone interested, I just ran a report of my interactions over the last 15mos. I averaged them over "21 working days in a month" and counted one week out of the office."
(It's total # / average per working day)
Total chart Interactions: 12956 / 41
Prescriptions: 2585 / 8.2
Appointments/video calls: 2767 / 8.8
Tasks : 4254 / 13.5
Attachments: 12853 / 40.8
Lab Results: 696 / 2.2
Calls (on my cell) : 1712 / 5.4
SMS Messages Emails: 16359 / 51.9
Emails: 3354 / 10.6
------------------------------------------------
Dr. Silakoski's Introduction Video






Resources Recommended by Dr. Silakoski
- Atlas MD EMR
- Doxy.me video communication platform
CONTACT:
Website: North Idaho DPC
Phone: (740) 339-9087 (call or text)
Message: FB Messenger
----------------------------------------------------------------------
TRANSCRIPT*
Welcome to the podcast, Dr. Silakoski.
Thanks. I'm so glad to be here.
It is so cool to talk with you because and I was saying this before the interview, but my dad also was at Fort hood. So thank you for your service to the country and thank you so much for being on the pod today.
Thank you. Thanks for your family service. And thanks for having.
So you grew up in Ohio and then you made your way to Fort hood, Texas, where you served as a soldier and a physician, and then you ended up in Idaho. So I wanted to go back to first that transition from Ohio to Fort hood. And I wanted to ask what led to your decision to serve and especially to serve as a physician in the U S army.
It's an interesting story. I will date myself when I say this. I was in high school when nine 11 happened and I felt I needed to serve. It was just something that I wanted to do. And, And I thought about going in right after high school and then decided I should get a degree first and go in as an officer.
So I started college and then forgot about it. As I decided I wanted to go to medical school. Then when I learned that there was a scholarship offered for med school through the military, I just applied for that and got it.
So when you got into the army and were an officer and a physician, what was life like at Fort hood for you?
It was a little different than I expected. I expected it to be more army and more military and less corporate medicine, which is what it ended up being the military at that time modeled their system after Kaiser Permanente and it was RVU tracks and.
Encounters per year generated or seen. And it was just see more patients in less time with less resources, always meeting the metrics. And I, I hated it. I decided I didn't want to be a doctor anymore very quickly.
It's so sad because just knowing the journey that is in front of you when you were a pre-med dreaming about medical school and it's, you know, the big, shiny pearly gates that, that you aspire to achieve.
And then to hear you get to the point that you are a physician and just saying, if this is. What I envisioned medicine to be that's really sad. And so I want to ask you on that point, when you talk about this corporate medicine model, that when you say Kaiser Permanente, I know exactly what that means living in California.
But when you described that, what was your day to day clinic experience like? And what were your duties like on an everyday basis?
It was, it varied vastly every couple of years, the military changes your location or your job. I was fortunate enough to be at Fort hood for the majority of that time.
And after residency, my four years of continued active duty included being a medical director for a community-based medical home that served about 8,000 enrollees who were retirees or family members living. And I had a couple of physicians that would come and go and a bunch of mid-levels that I was in, in charge of.
And it was a lot of chart review and administrative type work, but not enough time to do it. We saw 20 patients a day, which is on the low end, actually. You know, if If I think if I were other places, it would be more, but I still had to take time off to do PT tests and take time off to do, go to the range and take time off to go to TD wise temporary duty stations to do trainings, I had to go multiple times for between two days and two weeks to DC or San Antonio, or just multiple different places to get extra credentials and more things like that.
I had to help with getting our medical home PCMH certified. And that was not easy. But on a day-to-day basis, it was seeing 20 patients and then reviewing charts and just a lot of administrative stuff. I eventually became the medical director for the residency clinic. And that was even worse because the expectations and requirements were so unrealistic that it just drove me down.
It was. It's just
crazy just to hear the similarities between the fee for service job, that is not in the military and to hear your experience
for me, it's unexpected. So yeah I
didn't expect it to be like that. I guess I wouldn't have known until I got there and did it, I'm glad I did it. I'm glad I got the experience. I don't think that I would have the guts to do something like this if I hadn't gone through that, probably.
It gives you a lot of self confidence, I'm sure. In the ability to do or take on anything, if you can handle all of that on your plate. in terms of direct primary care between when you were at Fort hood and going to north Idaho DPC, how did you come to learn about
DPC?
Oh my gosh. Interesting story. So I decided I hated medicine and I was going to quit and my husband said, Jenna, you can't quit. We have too many student loans. So I said, what else can I do? I can work for the insurance companies, which are what got us into this mess in the first place. So that's out. I could try pharmaceutical.
Don't really want to do that. I didn't want something big. I know that because I. When things get too big, you lose the value. And so I said, what else could I do? I could do a different residency. I could do academics. I've already done that. I don't like it anymore. I used to love it. Then I learned about DPC.
I heard someone talking about it on an elevator. So I went and started looking about it. Yeah. I found the DTC group on Facebook, which I think everybody knows about at this point. And I just started reading and reviewing and saying, okay when I get out of the army, when my commitments done, this is what I'm going to do.
If I stay in medicine, this is what I'll do. So I started building a business plan and I was going to just start my own practice when I got out slowly and work, urgent care on the side. But then in 2018, as luck would have it, I had this amazing opportunity and I bought a medical practice.
That's amazing.
So tell us more because finding a medical practice on Facebook that definitely, if people weren't really tuning in at that point, I just want to emphasize, you just said you bought a medical practice on Facebook, so please tell us
I love it. Okay. So it really wasn't quite like that. I mean, It was, I met this gentleman Dr.
Richard Samuels, his name, amazing family physician. I now have come to know who was. Interested in selling his practice because he was going to be retiring in the near future and was looking for someone to come in and take it over like this. So my husband and I, right after interviewing at two rural jobs that were offering $250,000 a year, we drive, we flew here and we met him and his family and we saw the practice, met the employees, saw the area, fell in love and said, this is it.
I had never even heard of quarterly in Idaho before. And we don't have any family here. We had two very young kids, two dogs, two cats, all of us picked up and moved to north Idaho. I mean, We had a business valuation, hired attorneys, got a CPA, things like that. So we did it, I think we did it right. And I'll say six months into that.
Transitioning period. He had to retire earlier than expected due to some health concerns. It ended up being me alone with all of these patients. I was terrified, the attrition rate I was already worried about because you can't buy contracts. I couldn't buy patients. So I was paying for the name of the building of the practice and I was paying for the minimal amount of equipment that we would have as a DPC practice anyway.
And so I was terrified and worried and it turns out my attrition was, I think about 3%. It was so low. Patients number one, didn't want to go back into the system at all. And number two, they knew the staff and the employees and that all stayed the same. So I think that they felt really comfortable.
That's
amazing when you. We're starting. And you explain how over the six-month period he had to retire early, how was that for you in terms of onboarding all of those patients as your own.
Oh let me tell me, I thought it was going to go. I thought that I would get here and in, within maybe three months I would learn, hit the few he had kept at about 400 because he knew he was going to retire and he wanted to transition that over.
So I thought I would come and I would learn these 400 patients really quickly in the first three months. And I'd be good to go. It did not go like that. No, it was a lot harder than I expected. But I think it's also because I talk a lot, probably too much. Instead of having a person in, for an initial visit where I'm like, Hey, I'm the new doctor?
These are your medical problems. Yes. These are your meds. Yes. Okay, great. I'll see you when you need me or see you for your physical. I would see them for like an an hour and a half and chat about their family. You learn over there in front of them. So that might also have something to do with why they didn't want to leave.
I hope.
It totally worked out in your favor and even just your intro video on your blog when you joined the practice. It's just, it's so people can hear your voice, but it, that video was so personable. And so I'm, I'm assuming that broke down a lot of barriers or anxieties about having a new doctor at their DPC.
I hope so, because I really do think of my patients as my family and I want to know them and I want to serve them. I want to work for them. There's no middleman. I don't want to answer to their insurance companies or the administrators telling me how long I have to see them. I want to work with them only with them.
And it's just us. It, I, I did have a couple people leave because I was a young female and they wanted, you know, they were used to the older male and that's fine, much rather a female deliver my babies. Then, my male colleague, I don't want him to see that, So I understand that I did have, I've actually had two or three men say, I was going to quit, but I decided that since you were army, I'd give you a chance.
And I'm really glad I stayed. And that made, that just made my day. I'm glad that they can feel comfortable and I can have some things in common with everybody.
Definitely. And right now, what is your patient population like?
it's so varied. I do cradle-to-grave my youngest patient right now is about four months.
And my oldest patient is 92. I have a mix of I break them up like this there's government, which is Medicare Medicaid. That's about 15% or so. There is private insurance. Like all the BUCAs blue cross, all of those. And that total is about 50% and then the other 50% is cash paying or health shares.
And so I lump those together as well. Gotcha.
And in terms of the staff, you mentioned you had the staff come over with you, , who was at the clinic before, who has stayed on
with you? All of them, luckily and that was our receptionist. Kim she is amazing.
Knows everybody when they walk through the door, it is incredible. She can look at a phone number and know who it is on the caller ID. Oh my gosh. That's another reason it's so helpful. To keep someone on who already knows a lot of the patients and Rebecca who was receptionist slash medical assistant in Idaho, you don't have to have an inmate certificate.
So Rebecca happened to be Dr. Samuel's daughter and she is in credible. I mean, Kevin, Rebecca are both incredible, but Rebecca very quickly took on a lot of responsibilities because I didn't think it was going to be as hard as it was to learn all of these patients and, do everything medical wise.
I thought it was gonna have more time. Also not really putting weight on the fact that I had a two year old and a four month old at the time, but that made it a lot harder. But she immediately took everything and just started running with it. So she just she's the manager now.
And she is incredible. I can do everything. Yeah.
Going back to the transition when you were coming on as the primary doc and Dr.
Samuel was leaving, how did that go with Rebecca and with Kim in terms of, you were really new to them still, and they were going to be your team going into the future to continue taking care of the patients. How did that work in terms of. Them getting on your side, to talk you up in an amazing way to patients as they were getting their, get to know you visits in with you.
If I was Florida, how well it went, I was so surprised. I was really worried about that because not only were they there and Rebecca was his daughter, but also his wife works there. It was still, and she's still there too. She's a part-time counselor, which is included in our membership. And so I was really worried that family dynamic wouldn't allow for, or support an outsider.
And I was unbelievably wrong. I could not have asked for a better crew to come into. They were supportive. They were so helpful. Just teaching me about the area and the things I didn't know. And the specialists. I never had to do a prior auth in the army that I can recall. I don't think or I think people always did these things for us, which was great. But again, that's what drives up a lot of the overhead. And so they were, they accepted me and I think that they were probably just as fearful. They were probably like, I'm gonna lose my job and I'm going to, is she going to be nice? Is how is this going to change? Because he did things with very different.
He was very old-school a lot of, he kept double records with patient with record, paper records still in addition to their online chart and he he was very, is very meticulous very detail oriented. He is an incredibly brilliant man. And had he been in my spot, he probably would have been able to do everything by herself.
But I, when I came on, I couldn't do that. I just started handing stuff to Rebecca. And they accepted me. I think Rebecca is my age. So she and I are very much similar she's way more tech oriented than I am, but we're at least on the same page as we don't need to keep double records of paper and, things like that.
Oh, they were doing paper faxes. We changed it to entering facts, facts and so Kim, she was more Dr. Samuels generation and it was I think, and she's also like me and technology. We are not good at technology we need for Becca, but she has an incredible knowledge of people and she's so personable.
Everybody just loves her so much. . And I'm so glad that they were willing to stay.
And I want to ask about finances because with you having moved to buy a new practice and just the. When you talked about the CPA and the lawyer and all the costs going into Ben, buying the practice and then paying yourself and paying your employees.
How did that all work for you in terms of, did you have to take out a loan or what did
that look like? I did. I took out an SBA loan. Now looking back feel like I I got an incredibly good deal on this. We had spent most of our savings because we had to put down payments and we had to travel here several times.
We had to hire attorneys. And so if patients quit, then I wasn't going to have a paycheck and I wouldn't be able to pay the loans. So that was a little scary. But the bank here, they were incredible. It was a regional bank and they didn't know me from Jack. You know, I'd been in the military, I'd never owned a business.
Like I'd never even been a, civilian doctor, but they were like, yeah, you'll probably be fine. Doctors. Don't usually default on their loans. Here's a house loan, here's a car loan. Here's your practice loan. And here's a line of credit. I didn't use the line of credit at all and didn't ever need it.
No, it was good. Things sped up incredibly fast. It went faster than I could have imagined. I'm now bringing on a partner at the end of the year, Dr. Odom is going to be here in November and we are so happy to have him. He and his family are incredible. And patients are just like knocking down the door.
I just can't keep up with it. I'm exhausted. Regarding finances. It, the practice was generating about a paycheck of about $10,000 a month for the doc at that time. And that was that was enough to pay the loan and the bills and things like that.
So that was great.
After getting your finances. Situated and knowing that you had staff to pay, but the patient population hadn't really changed much. How did you go about benefits? Did you have benefits that you were paying that were already established for Rebecca and Kim and
Yeah. They at the time they had an option for a simple IRAs and that was pretty much it and a membership to the clinic.
They were allowed to have medical care. I would like to consider paying for a membership at a different clinic. We could just, because I think it's a little easier. You can have more objectivity if you're not their employer and their doctor. But so I restarted the IRA and I do bonuses, holiday bonuses.
And I do three weeks of PTO six paid holidays federal holidays in addition to the three weeks. And so far, that's it, I'm looking at dental and either a catastrophic plan or something like that for the future. Awesome.
So as you got your feet established, as you became the solo doc, did you experience much growth after having onboarded those 400
people?
Oh my gosh. My average was about a net gain of, I think it was a net gain of seven a month for the first, the next six months. And then in January and February, I was averaging 25 a month. So I just couldn't keep up with it. So I closed my panel at about 5 65 and just let some attrition happen with people moving or dying, things like that.
And so now I'm about 5 55 and I've opened it back up again, but I've got a huge waiting list and and I really want people to go to Dr. Odom because I wanna, talk him up. Say how amazing he is. My attrition rate is probably about, I haven't calculated it this year yet in 2021, but from the time I opened to the end of 2020, it was about a little over 1%.
I was like 1.3%. So I think it was pretty good. Incredible. Yeah.
Now I have to ask, with having a two year old and having a four month old. When this all started, how do you balance family life now that you have over 500 patients?
So I now also have a virtual assistant who is very helpful, but I am trying, I am not good at setting boundaries at all, but I'm trying very hard to do that when I'm at work. It's work time when I'm at home, it's home time. I put my phones away. I put, you know, I leave the ringer on, in case there's an emergency, but I put everything away and I try to be present at home.
And I'm frankly, I was working 60, 80 hours a week in the army. I think that I only work about 35 hours a week, but my husband would beg to differ. I think I love it so much. I just want to do everything and manage
that love of working. On the business rather than working in the business.
It really is something that a lot of DPC doctors have said in terms of on the podcast and just in personal conversations that you're working harder, but it's not working harder to the point of burnout. It's working harder because this is a baby and you love it. So that's amazing.
Yeah. I don't foresee burnout in this position because everything I do is just a little bit different every time.
And it's always something for me that I want to do. So if I don't think it's important, then I'm just going to say, no, I'm sorry. And I don't have a boss to answer to, to tell me you have to do this and you have to meet those metrics. And I'm going to just say, Nope, not going to do it.
When you speak of boundaries, I want to ask, what words of advice would you give to others who might be challenged with setting boundaries with their practice or with their patients or both?
Um, I would be a really bad person to ask those people who can do it and need to tell me so far, what I've found is saying upfront and being very clear during the meet and greet to say, I am not a concierge doctor. I think that there is a big difference and I have a family and my family is very important.
I'm human. I will be available for you. I will get you in very quickly. I will answer your texts during business hours, but after hours, my kids, my family, it's their time. And they have been incredibly respectful about it. I'm the one that breaks the boundaries. Cause I know when they text me and they say, I need a refill on this.
I know that it can wait until tomorrow. I know that I can't, I just can't let it sit there.
Awesome. Now previously in one of the DPC docs feeds you had written, I just ran a report of my interactions over the last 15 months.
I averaged them over 21 working days in a month and counted one week out of the office. So the total number per average, per working day.
So I, it was total number of whatever it was. And then afterwards was the per day. So if I averaged it over 21 working days over that year, it would be so like, if I saw a hundred patients that year, and I only worked 10 days that year, I would have averaged 10 patients a day. Gotcha.
So these are some amazing pieces of data, because I think that this is where even though, you talk about that.
You're not the expert of boundaries. I think that this is a huge step in the right direction to taking control and holding the reins, so to speak over your business, because you're actually knowing where your time is going. And so one I wanted to ask, how did you get the data that we're about to talk
about?
I pulled it from Atlas MD, the EMR. That's the one I use. I switched when I came on, we were using practice fusion and I liked it, but there was so much good about Atlas that I decided to make that switch. And it is really hard to switch EMR.
Just delving into that right there. How did you guys, as a team make that all happen and how long did it take?
It took, also took longer than I expected. Atlas support was really good in getting all of that moved over. So it all went over in as PDF files and attachments. But it took, I think a couple months maybe. it was a little more intuitive and there were so many good things about it that it was really easy to just kind of transition from the, for me, it was because I didn't hadn't used practice, fusion that long for them.
It was a little harder because they had used it longer, but it was quick. It was probably within a week or two. It was pretty routine, I think.
Nice. Now for the data the big one. That I gleaned from your list and I'll post the rest of the list on the, on your accompanying blog. But total chart interactions was 12,956, averaging 41 per day.
And calls on your cell phone 1,712 averaging 5.4 a day. And SMS messages, 16,359 averaging 51.9 a day and emails 3,354 averaging 10.6 a day. So just from that amount of data, your practice seems to be very heavily technology capable.
One in there. People love to communicate with you. It seems through messages, on text. Was that representative of what the patients were doing before you came on?
No, it transitioned. They, it was very traditional, so he converted his fee for service practice to DPC.
So it was very traditional. They would call their desk, they would make an appointment. They would come in and talk about things for up where I texted them. Hey, your labs were normal.
when you set the time aside, like you mentioned before about this is work time, this is family time.
What portion of your day? Do you spend doing the communication and do you have a set time for that or do you do it throughout the
day? I just do it throughout the day. Usually I have admin time, but usually before my first patient at nine and then admin time after my last patient at three 30, but I'm usually walking through the door at five till nine, and I'm usually out the door right after my last station.
So I have to do it during the day prior to the pandemic, I used to take an hour and a half lunch. So I'm in the office now about nine to five. And I do a 30 to 90 minute lunch depending on the day at this point. And a lot of this data is from six months worth of pandemic too, because I did a lot of telemedicine during that time.
So there was a ton of video calls and text messaging and things like that. And so I try to just work it in throughout the day, to be honest, I'm not good at that kind of thing. I'm not good at. Oh yeah, I gotta check the email. Oh yeah, I got this. So my assistant helps me with that a ton. And so we regroup, twice a day or so.
And she says, Hey doc, this came in, in in this case, she's an RN. This came in, this, came in, this, came in, this, came in, these were the results. Do you want me to file these? And I now have an incredibly great filing system and Atlas that I love. So for people who use Atlas and haven't found their thing yet if you're interested in mine, I have five categories.
It's labs, pathology images, consults, and records, I think. And so it'll be like image, colon, CT, parentheses, normal slash date slash patient name. And so when I'm looking for something very quickly, I can just quickly scroll through, oh, I need that image. There it is. Or I need that consult. Oh, there it is.
This is what I love about the idea that if you've seen one DVC, you've seen one DBC because I'm sure you just helped a bunch of people with regards to. Learning a new way to organize their EMR. So thank you. That's amazing. Now, one of the things that I'm laughing at in your data, it, because I had 63 messages in one day on, in my fee for service box, but your lab results, you had 696 over the 21 day period.
And on average 2.2. Okay. And I'm just like, that's amazing. So could you talk about, how you seem to get that number in it because that's
just, that's almost a dream. It okay. That's another thing is I don't have to order a ton of labs for people who don't need them. And I have time to explain why they don't need a lab.
I also. Don't have that many patients. you know, In a fee for service world where a panel is 2000 patients or more 4,000 patients, even sometimes I don't know, I'm thinking if you get 1% of labs a day, that's a lot, you can't keep up with that. It's impossible.
I've never seen a day that I had only
2.2 labs in a day.
So amazing and appointments. That's a big thing for those people who are interested in DPC, but are like how many do you actually see in a day you had 2,767 and 8.8 per day on average. And so can you explain how you do it so that you're not seeing the 20 patients a day? Like you weren't?
Yep. My panel at Fort hood was a lot bigger. My panel was. I can't remember now 1200 or 1800 or something. And I was seeing other people's patients for urgent needs. So I think a lot of it is also, I don't need someone to come in and pay a copay so that I can bill something like a 9, 9 2 1 2, just to go over normal labs.
I don't care about that. I'll text them and tell them their labs are normal. Or um, things that don't need an appointment. Patient called me that I hadn't seen in a while said I need a refill on my blood pressure meds. And I said, well, I haven't seen you in awhile. How's your blood pressure doing? And he said, actually, I haven't been taking it that often. Let me take it right now. Oh, it's 117 over 70. Perfect. Glad, you know, it's going well, no symptoms. Here's your refill. Call me if and when you need me
and you're totally accessible.
If, and when he needs you.
Yeah. So many people just walk in off the street. One, one guy came in, knew that I would be furious with him because his blood pressure was 180 over a hundred. And I said, what in the world happened? And he said I haven't taken my meds for a week. Okay. Yeah, that'll do it.
Why haven't you been in well, I knew you were going to be mad at me, so I said let's get our meds restarted and see how your blood pressure does. Oh
my goodness.
I, I think about how like being in a small town, I have totally had those reactions where people will talk to you.
Like you're a family member. Like you treat them like a family member. But that's, it's just something that somebody who is in a panel of 2000, a panel of more than 2000 that, do they know that doctor, do they expect that type of relationship with them? And
you can't know that many people it's not safe.
Yeah. And I look back on my own panel and for some patients I'm like, I haven't seen this person in four years, so how am I supposed to know, everything that happened. And so I am glad that your patients, know who you are and they are keeping in mind, that you actually care about them because even the idea of him thinking that you would be mad means that he knows that you care.
Yeah. I had another set of patients, a husband, and a wife who I didn't think they liked me at all.
I thought the wife liked me. Okay. But I thought the husband hated me. And I felt so bad. He had this new sudden onset dyspnea on exertion and some very stable angina type symptoms, not sudden onset, but progressive onset. And so I explained to him why it was important to get a stress test, especially with this family history, especially with obesity, blah, blah, blah, blah, blah.
And he was furious and I thought, for sure he was going to quit. And it turns out that I'm his favorite doctor that he's ever. And they invited me and my husband over for dinner and we're going to go, I think you do need to have boundaries and you can't do that with everybody.
But this is a small town and I'm a business owner and they're fellow business owners. And I just blew my mind. One very similar to that took his A1C, trusted me enough to get him started on insulin. He wouldn't even take Metformin before and I got him on insulin. Eventually he has lost so much weight.
He has come almost completely off of his insulin. And his A1C is in the sixties. It's amazing. It is incredible. There's no way I would've had time like that or that he would have gotten comfortable enough for someone to be able to allow them to. An injectable that's, it doesn't happen in when you're seeing 20 to 40 patients a day in most cases, I think
You shared the Dr.
Samuel was very much traditional and he had paper as well as practice fusion, but texting wasn't really a thing that patients were used to. So how did it go when they needed to use tech, like video calls in your practice during the pandemic,
there was a huge divide. They either loved it and were super grateful or they hated it and they wanted to be seen in person.
And that's how they'd always done it. And that is what they will do. Yuri is if I did a car side visit or furious that they had to wear a mask, no one here masks, no one in north Idaho MES. And they do large gatherings. A very loud minority or the majority don't care.
And in terms of your video visits, were you using video visits through Atlas or using a different platform? I
use doxy.me for the most part. It seemed a little more reliable. I not, maybe not reliable is not the right word. I don't know. It just, I, that was what I tended to use and it worked fine.
That's another thing, I guess in the army, I was in a sea Bernie unit, which is chemical, biological, radiological, nuclear, and explosive warfare unit. So we literally trained for stateside disasters, such as pandemics. And we had to be ready at a moment's notice to be deployed to a state side disaster.
And so I loved being able to make my own decisions about this and do what I wanted to do in my clinic, how I wanted to do it without having someone else tell me, I'm sorry. You have to reuse your not in 95 for a week, or, Nope, I'm sorry. You actually have to see all those sick visits. In-person. When
you were in that space of, wow, this is exactly what I trained for, and now I'm having to use it.
And I, I have the skills to design my own practice around this pandemic. What were some of the strategies that you put in place specifically so that you could serve your patients the best? In addition to what you've already mentioned?
My husband actually recognized it incredibly early. So December, he was like, Ooh, Jenna, this is going to get bad.
So we just ordered a bunch of supplies and we we inventoried them masked suite, estimated it at the rate. It was going in about March. It hadn't quite hit us yet. So I estimated how many sick patients we would be seeing and what kind of equipment we would need for that. And then I just extrapolated that but enough for a quarter.
And then every month we would check it and see how much we had if we were doing it. Right. And then we had sick visits had to be done by video first. They had to be triaged by them. Manager slash ma then they had to be done by video first. Then if they needed to be seen, it was car side in full PPE and only well visits could come in, but they had to mask and that was only if they demanded a visit or really needed it.
I recommended that they push out, especially since by that point, I had met everyone in new everyone, almost everyone. And
do you have patients who don't have internet?
Yeah. I have a couple. And
how did you manage
that? They don't have cell phones, so we FaceTimed or whatever.
Reflecting on your time at Fort hood, and just the fact that you were serving in the army, I'm sure that you were dealing with a lot of mental health issues.
And so I wanted to go back to the fact that you have, and you said included in your membership is our counseling services. So can you touch on that portion of your practice?
Absolutely. So when I decided that I wanted to quit medicine, it was when I was, I went through a very severe depression. The tipping point was when I had an emergency oophorectomy because I had a very large cyst that they thought was cancer. Thank God that it ended up not being cancer, but so I recognize it, not just in my patients, in the military, but also in myself. I can't get disability insurance now, despite running an incredibly successful practice and getting through medical school and being a doctor like who wouldn't want to insure that type of person.
But not only is it close for me just personally, but seeing it in my patients too. So I think that DPC can be way, way more than just. A physician patient relationship. So I pay a counselor, a part-time salary, and patients can make appointments with her and it's included in membership. She just uses one of the rooms.
I also would like to do this with massage therapy and a lot of other services as well. So I want to give them the space. I actually I'm closing on my building that I'm in. So my building has three units in it and I'm in one unit and there's an insurance in the other two units. And when that insurance agent retires, I'm going to take over the whole unit.
And I want to give this space away. I want to have people who will come in and see my patients either for free or at extreme discounted rate. And then they can build their own practice within that as well. They just have to see my patients and give them really good deals because give them free rent. So I I think there can be a lot more to it.
, oh, I've got to tell you one more thing too. I'm so sorry. Go for it. My long-term goal. So my 15 to 20 year plan is I want to have a network of direct insurance lab path radiology, and I'm missing 1 35 path uh, pharmacy. And I want to have a direct care network that the insurance would more be more like a cooperative health share type thing.
But I want to be the CEO of this company and pay myself no more than the lowest paid person of my company. And I want to set an example and I want these to be for direct care doctors. I want direct care physicians utilizing this only for their patients. I won't, it won't be for anybody else. And it will be them getting it at cost or just like maybe 10% above costs.
And. Then I'm going to take out a third middle man. I'm like, I'm not going to have to buy from a wholesaler because I'm just going to give it to the patients, or you wouldn't have to buy it from a lab Corp because you would just send me the blood and I would run it for you at my cost.
So if I'm paying lab LabCorp $5 for a CBC, it probably costs them a dollar to run. So then it's only costing you a dollar by that point. I don't want to make a profit on this. I want this to be, I've got to make my money doing something else. I don't know what, but it's going to be non-profit and I'm going to try to set an example for how healthcare should be in our country.
just, hearing your story from where you were at Fort hood to taking over a practice and then dreaming and planning already for the 15 to 20 year plan. It's just incredible. I just. Could you even imagine that's the, this is the space that you would be in when you were in those days of seeing 20 patients and supervising mid-levels and taking care of having to travel as well as be your physician at the base.
It's just incredible.
And to travel, you would have to fill out like eight pieces of paper and take them to all kinds of different departments and have different signatures. And they were only open on Tuesdays at noon, or it was awful. It's impossible, but yeah, it's it's, I have gone a complete different direction in my life and I could never have imagined this and I couldn't be happier.
I think every doctor deserves this.
now I want to ask, because. With every doctor and I am totally with you on that. And every doctor deserves this because this is allowing us to fulfill our calling to medicine and to be able to do the things that we want to do for patients the way we want to do them for patients.
But with you adding Dr. Odom in the fall, I want to ask about now, how did you find Dr. Odom on Facebook? Did you find Dr. Odom a different way? How did
well on Facebook? So I have a friend who I went to residency with Dr. Pierre's her name? Fiore, Dr. . And she called me up one day and said, Hey, Jen, I have a friend here, colleague, who has been interested in DPC for awhile.
He's been thinking about it for a few years and he's getting out next year. He'd like to talk to you. I said, oh, I'd love to talk to him. So he called me up and I said, I w I felt like there was a really good connection and that we could work well, he's also, he's in the air force. So he's also a military, he gets the lifestyle and everything.
And so I said let's just say we partner. And he was like, I don't even know you, but it turns out he came here for an entire month. And he saw the area, met a ton of my patients and I asked them upfront. I said, I'm having him here to make this offer. I want him to work with me and us cover for each other if, when I'm ever on vacation or if I ever have to call out, so there's a doctor in the office.
Most of them were like, yeah, he's great. He's amazing. We loved him and select fewer. Like he told me I needed to lose weight and stop smoking. And I was like, you do. But yeah, it was, I forgot where I forgot what the question was. How did I meet him through a friend, a mutual friend, and now they're coming in he's with his wife, they have twin four year olds are I think, all about to be five or just recently turned five.
And yeah,
when you were like this could really be my future partner. What were some of the questions? Because you had excellent questions when you decided to buy the practice, what were some of those questions that you had for doctors?
We got to work together for an entire month.
So I saw him every day. I learned about his personality. I learned what his goals were when his aspirations were I feel like he is a more detailed oriented person and I'm a little bit more of a 10, 15, 20 year planner. But I asked him things like what would you do if this happened? And he was, he also asked a lot of those things like Jenny, we have to plan for everything.
You never want something to fail, but what if it did, what if we worked together for a year and we don't like each other. And so we just talked about those things, like how we would split patients, what would happen? Would it be amicable? You know, All of the I'm pretty outspoken. But I also love people.
So if it doesn't work for someone I'm not going to force them to stay, I don't, and I want it. I want them to be happy. I want everybody to be successful. Yeah.
when he comes on, will he earned his keep, so to speak based on the patients that he is accepting off the wait list, or is he going to be employed?
How is it going to work out? I
can, I'd be happy to send anyone the contract. He wants to look at it, but I'm doing an, a guaranteed $8,000 a month salary for 20 hours a week average of 20 hours a week. And after that, we, I think it said we split like every 50 patients, 50 will go to the practice and 50 gold go to his salary until he reaches.
I think we said six, five or 600 patients. Um, and my goal for us. And we'll talk about this and, figure it out for sure. But I would love to be making $300,000 a year working four days a week. And. I have a full practice.
while we're talking about numbers, what is your overhead
overhead right now for me is high because I'm doing a lot of marketing and just prepping for getting him on board.
I would, I think it's about 40%. Let me see.
Yeah. It's about like 38%. Gotcha. And,
When you look back. The idea of buying a practice again, do you have others reaching out to you who are asking about how you did it or asking for advice as to how to buy another DPC? If they're looking into that,
I had a couple people ask about that and I just tell them my experience, how much I paid, how much they were asking, how much, what kind of questions I asked and if it was a good thing or not.
And most DPC practices, I feel aren't for sale either it's partnership or something like that. I've only seen a couple for sale, I think.
in terms of you being in practice since 2019 and being in the position that you are having bought a business, what are some of the questions that you get most frequently from those who reach out to you?
Can I do it. Is it possible? I don't think it's possible. And I tell him it is incredibly easy to make it possible. You were brainwashed. Doctors are brainwashed. I say to someone, if they call me up and I just ask them, I say, okay, how much money do you want to make? I'm not sure. Maybe I don't know, 180,000 a year.
And I'm like you're undervaluing yourself, but let's see if you do 180,000 a year. That means, oh, and I also ask how many patients do you want to see a day? Okay. How many days a week do you want to work? Okay, well then your patients are going to have to pay this much per month. And it usually ends up being like 75 to $90 a month on average.
And they're like I don't. Why would people pay for that? And I'm like P value. They love relationship. They want something to value people. And that's the kind of person you want as a patient. You want the people who value you as a person. You are not a cog in a wheel. You are not. We're brainwashed.
You're not, you don't need to be working for a company or a corporation. They're making like $1.3 million off of you a year about, and they're paying you 150 or $200,000 a year and they're working. You like a dog. Why not make more and work less and make more
it's doable.
For those who can relate to that experience or that feeling that you described when you were in that corporate army medicine to now, it's just, it's so inspirational. So I, Those words our words to take to heart and And just insert into your potential future dream, your future, 15 to 20 year plan.
If you are on the cusp of thinking about DPC,
I've literally never been happier in my entire adult life. I never thought I could love this much ever, not even in med school, when I was having dreams of what I thought medicine was going to be like, I went to the, I went to the Philippines on two mission trips and I was like, this is amazing.
People are grateful. They're thankful. They're they listen to what you have to say. They want to hear what you have to say. And I thought it would be like that. And it was not, it was a lot of paperwork, a lot of administration, and now I just couldn't be happier.
Can you describe your most difficult day and DPC best far?
I like to say that, and this is not really a description of my day per se, but my worst, hardest day in DPC is about 40% of what my average was every day in the army.
Incredible.
Yeah. And so sad. I really can't think of a worst day. I mean, I remember a couple of times just tearing up at the end of the day, being overwhelmed, thinking well, I'm worried about this person and I've got so many orders to put in and, just normal stress, I think.
But nothing like what your normal stress is in the day-to-day corporate job, I think. Yeah.
You know that it highlights that reality that a lot of us face where even a fee for service, when we are with patients, we love it. It's when we step out of the room and when we have to do all of the other things and when we're restricted on doing certain things, that's where I think a lot of that burnout comes from.
And so the idea that you're just always in that patient relationship place, it's just, if people think about it in that context, like how with you sharing, how you are living in that space. It just really paints a different picture of her people and
the big picture with this podcast is to share how everybody is doing it their own way. And you can take best
practices and you will find someone who you can connect with and who did it like you want to do it? I love it.
So now going on a roller coaster ride, what is your best day in DPC?
The best day? One of the best days is a patient who called me and said, I. I don't have any health problems. I don't have anything wrong with me. I just need to get this referral for my mild sleep apnea. I need this dental referral, so my insurance will pay for it.
And my doctor won't get me in. I've been trying for months. And I said, okay, no problem. You sound legit. So I did a quick video, documented everything, talk to her about her problems or medical history, send the referral. Then her mammogram came back to me the next day and said malignancy.
So I had not yet seen this woman in person and I called her and I had to tell her, I'm really sorry to have to tell you this, having not met you, but your mammogram actually came back as concerning for cancer. And I want you to meet me at the office. And so we had a discussion about it. I got her in for a biopsy.
She had the biopsy and the results and two specialty consults scheduled before her other primary care doctor called to tell her about the mammo results
as it should be right as
it should be. Yeah, that's crazy. Wow.
There are too many good days to even remember them all. I, there's so many that are going through my head and I'm like, I don't want to tell this story and I want to tell that story. I want to tell about this patient. I want to talk with this person. I love my patients so much.
And one of them, I was sick this past week. They brought me, or they sent flowers, Rose Bush to my office. And it's beautiful. I'm so thankful. So many texts and well-wishes, it's incredible.
And I hope that you take pictures in the next 15 to 20 years of that Rose Bush and just see how it flourishes, just like you will.
Jenna those who wish to reach out to you after this podcast, what is the best way for them to contact?
You can text me on my cell phone and it's (740) 339-9087. Or message me on Facebook.
Thank you so much, Dr. Silakoski for joining us today.
Thank you for having me.
*Transcript generated by AI so please forgive errors.












Comments